The global stage of the United Nations General Assembly (UNGA)...
Read MoreSTRENGTHENING PRIMARY HEALTHCARE (PHC) SYSTEMS PROJECT
We are building a resilient and efficient healthcare system through improved management capacity and enhanced M&E systems.
A strong health system is critical to achieving universal health coverage.
The Primary Health System remains the cornerstone of the health system, with the Primary Health Care (PHC) as the first level of care, the entry point into the healthcare providing basic primary care services.
Strong health systems go beyond making services available – they ensure that quality services are delivered in an effective, efficient, and safe manner for health care workers and communities alike.
Our PHC Transformation Intervention has helped improve overall health outcomes by:
- Increasing PHC output and boosting productivity
- Saving hours in operational time and labour
- Reducing operational cost
- Increasing client and community satisfaction
Despite significant investments, the primary healthcare (PHC) system continues to perform sub-optimally with issues around governance, management, financing, and monitoring.
While there have been several efforts to ensure the availability of critical primary health services, evidence suggests that critical gaps, such as weak PHC governance structures, inadequate staff capacity to effectively and efficiently manage PHC operations, and poor data documentation and use for decision making, continue to hinder the provision of essential health services and lead to poor maternal and child health outcomes.
These gaps often manifest as:
- frequent drug stock-outs
- high level of PHC staff absenteeism
- low quality and perception of care
- low level of trust for PHCs amongst communities
- ineffective use of scarce financial and non-financial resources.
What We Do
Sociocapital, through funding of Technical Advice Connect, implements the Strengthening Primary Healthcare (PHC) Systems Project in Nasarawa State, Nigeria, to demonstrate the feasibility of enhancing PHC services through improved management capacity and data systems, ensuring accessible and quality healthcare for all communities.
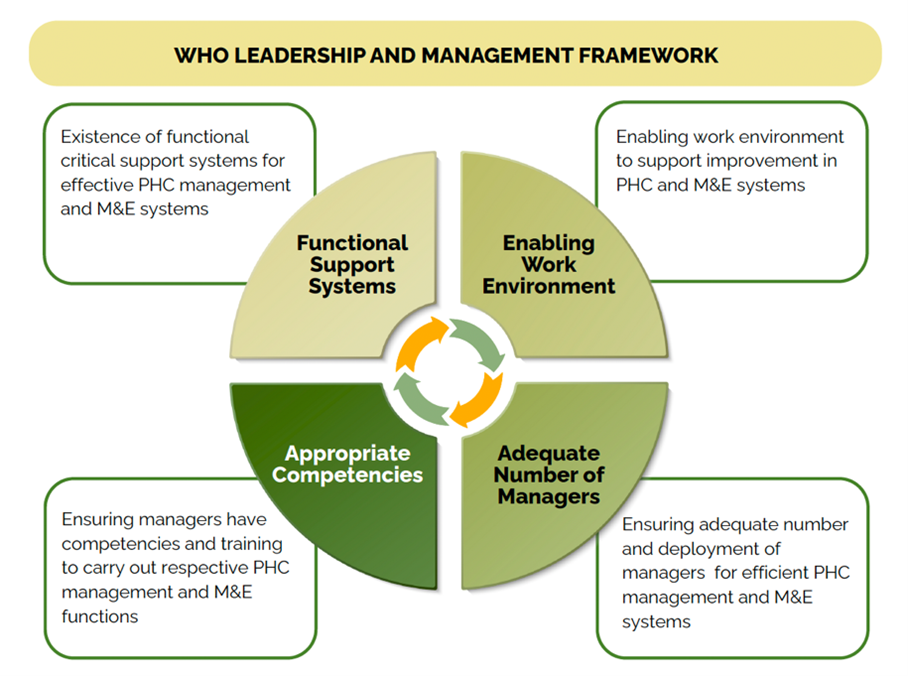
The Project promotes sustainable health systems at the primary health care levels through a set of tailored interventions to address gaps across 4 themes of the WHO’s framework for leadership and management as it relates to RMNCH+N.
How We Work
We work with the State government to improve the functionality and effectiveness of Basic Healthcare Provision Fund PHC facilities, ensuring better community health outcomes.
We do this through:
- Landscape PHC Management and Data Management domains to identify weak links and customise evidence-based, culturally sensitive solutions to the identified gaps
- Integrate evidence-based solutions within government operational plans and budgets
- Work with local training institutions to integrate PHC Training Programs into preservice and in-service training
- Government-led coordination platforms for PHC management & governance with partner buy-in.
- Design and distribute low-fidelity, reusable Facility-level Runs Charts
- Establish Online Dashboards for PHC Management review and course corrections
- Consolidate existing investment for articulation within health service delivery plans, consistent with existing PHC improvement efforts.
- Engage different governmental, community, and development partner stakeholder interactions and actions needed to sustain PHC improvement efforts
- Government-led coordination platforms for PHC management & governance with partner buy-in.
Insights
Project Report

Towards Transformational Primary Healthcare Service Delivery
This report summarizes Nasarawa State’s progress toward improving Primary Healthcare (PHC) to enhance PHC services through improved management capacity and data systems. The intervention was funded by the Gates Foundation.
Technical Brief

Health Information System Strengthening for Evidence-Based Decision Making
Monitoring and Evaluation (M&E) is central to effective health information systems and evidence-based decision-making. This technical brief explored how we champion the culture of documentation, real-time data use, and accountability, to: Improve data-informed decision-making; Enhance advocacy and planning with evidence; and Strengthen health outcomes through system resilience
Technical Brief
Strengthening Workforce Accountability in Primary Health Care Facilities
Unapproved absenteeism undermines productivity, disrupts operations, and affects patient trust. This technical brief documents how, through mentoring, coaching, and supportive supervision, we used data and design-thinking to reduce unapproved and equip communities to ensure greater, more transparent healthcare worker accountability.
Read Our Blogs/Articles
Towards Transformational Primary Healthcare: Lessons from Nasarawa State
Towards Transformational Primary Healthcare: Lessons from Nasarawa State “Strong primary...
Read MoreStronger Systems, Stronger Care: How Nasarawa is Reimagining Primary Healthcare
Stronger Systems, Stronger Care: How Nasarawa is Reimagining Primary Healthcare...
Read MoreResources

PHC Management Competency Framework
The PHC Management Competency Framework provides guidance on core values and competencies required by health workers to provide quality client-centered services at the different PHC levels. It also highlights job descriptions for key health workers operating at the PHC with detailed standard operating procedures (SOPs) and checklists to guide service delivery.

PHC Management Competency Framework
A detailed training manual for health workers on effective management practices. The manual delivers a bouquet of essential trainings required to effectively administer primary health care delivery. An E-learning training portal is currently being developed.
Stories of Change
Staff Motivation Reducing Absenteeism Rates





Before this project, coming to the health center was often discouraging — medicines were not always available, and waiting times were long, and staff treated us poorly. But now things have changed. The facility staff are more attentive, drugs are available, and we are treated with respect. I feel safer bringing my children here, and I trust the services much more than before.
Delilah Dennis Community member, Garaku 1 Kokona LGAThis Project has been a game-changer for Nasarawa State. By embedding mentorship, stronger data systems, and practical management tools, we are not only improving service delivery today but laying the foundation for a more resilient and sustainable PHC system for the future.
Dr. Usman Iskilu Saleh Executive Secretary, Nasarawa State PHCDAProject Partners

Technical Advice Connect LTD/GTE (TAConnect) delivers tailored and cohesive technical assistance to strengthen health systems and enhance service delivery. Its mission is to support national and sub-national governments to build and strengthen resilient health systems and improve health outcomes.
Learn more at https://taconnect-ng.org/

The Nasarawa State Primary Health Care Development Agency (NAPHDA) coordinates and oversees primary healthcare services in Nasarawa State. It leads policy development, service delivery, and health reforms, partnering with stakeholders to enhance access to quality healthcare across 13 LGAs. NAPHDA also focuses on capacity building, monitoring, and implementing national health initiatives, aligning with Nigeria’s health sector goals.
Learn more at www.naphda.org.ng

Sociocapital Health employs evidence-based insights to address Social Determinants of Health Equity through strategies at patient, practice, and community levels, ensuring equitable access to respectful healthcare for underserved populations. Their mission is to eliminate systemic barriers to critical services and resources, fostering resilience and empowering communities to overcome poverty.
Learn more at www.sociocapital.org/global-health


During monitoring visits, we discovered high staff absenteeism of 35% weekly due to burnout and feeling undervalued. Through the introduction of a "Healthcare Hero" recognition, peer learning sessions, and structured feedback meetings, we paid attention to work culture. "Staff retention improved by 80%, unapproved absenteeism dropped to 0% across all facilities as of December 2024, and patient satisfaction increased by 40%."
Vera Yusuf PHC Mentor.